On June 2, 2013, the Sunday edition of the New York Times ran a major investigative
article by Elizabeth Rosenthal called “The
$2.7 Trillion medical bill”, with the subtitle “Colonoscopies explain why
the US leads the world in health expenditures”. It is a damning article about
the US health care system, and the fact – fact
– that our costs are much higher than those in other countries but our outcomes
are often worse, and large portions of our population are not even covered.
Of course, it is not all colonoscopies. Yes, the average cost for a colonoscopy in the US
is $1,155 compared to $655 in Switzerland (for example). And many cost much
more; in the first paragraphs of the article we hear about charges of $6,385, $7,563.56, $9,142.84 and $19,438
-- “…which included a polyp removal.
While their insurers negotiated down the price, the final tab for each test was
more than $3,500.” ! But the graphic at the top of the article compares US prices
for other common procedures with those of other first-world countries: Angiogram $914 US, $35 Canada; hip replacement $40,364 US, $7,731
Spain; MRI $1,121 US, $319
Netherlands; Lipitor (atorvastatin, a
drug to treat high cholesterol) $124 US, $6 New Zealand.
But colonoscopies
provide a good example for why we pay
so much more for procedures – and it is not because they are of higher quality:
“Colonoscopies… are the most expensive
screening test that healthy Americans routinely undergo — and often cost more
than childbirth or an appendectomy in most other developed countries. Their
numbers have increased manyfold over the last 15 years, with data from the
Centers for Disease Control and Prevention suggesting that more than 10 million
people get them each year, adding up to more than $10 billion in annual costs. Largely
an office procedure when widespread screening was first recommended,
colonoscopies have moved into surgery centers — which were created as a step
down from costly hospital care but are now often a lucrative step up from
doctors’ examining rooms — where they are billed like a quasi operation. They
are often prescribed and performed more frequently than medical guidelines
recommend.
The high price paid for colonoscopies
mostly results not from top-notch patient care, according to interviews with
health care experts and economists, but from business plans seeking to maximize
revenue; haggling between hospitals and insurers that have no relation to the
actual costs of performing the procedure; and lobbying, marketing and turf
battles among specialists that increase patient fees.”
Welcome to the
world of for-profit health care. Where the principle of “maximize profit”
determines what health care institutions do. Where “what we do” (our “product”)
is health care, but we prefer to do it on those with really good insurance.
Where we adjust our charges to maximize the difference between what it costs us
and what we are paid. Where the rules set by insurers or government with the
aim of regulating costs are seen as challenges to be gamed for maximum profit.
The movement of colonoscopies – and many other procedures – from doctors’
offices to “surgi-centers” is a great example. If performing colonoscopy in an
office was unsafe, moving to a surgi-center might be a good idea, but there is
little evidence that it was. Moreover, the increased price for performing a
procedure in such a center far exceeds the increased cost of doing it there;
the reason for the move is not
patient safety, but taking advantage of a loophole to be able to charge more.
Rosenthal’s
article is a long one; it extensively documents both the high cost of health
care in the US and the reasons why it is so high, which are rarely related to
quality. This is illustrated by an article published in the Times a few weeks earlier, “New Jersey hospital has highest billing
rates in the nation”, by
Julie Creswell, Barry Meier, and Jo Craven McGinty. “The most expensive hospital in America is not set amid the swaying palm
trees of Beverly Hills or the luxury townhouses of New York’s Upper East Side,”
they write, but Bayonne Medical Center, in Bayonne, NJ, where the average
charges are 4.1 times the national average
charge, not to mention what Medicare will pay. For some services it is much
higher: “Bayonne Medical typically
charged $99,689 for treating each case of chronic lung disease, 5.5 times as
much as other hospitals and 17.5 times as much as Medicare paid in
reimbursement. The hospital also charged on average of $120,040 to treat
transient ischemia, a type of small stroke that has no lasting effect. That was
5.6 times the national average and 23.6 times what Medicare paid.”
How can they get
away with this? Who will pay them so much? After all, if I can buy a Chevrolet
for $25,000 at one dealer in town, why would I pay $75,000 for the same car somewhere
else? Ah, but health care is different. For one thing, you might be sick when
you have to find a hospital to care for you, and you might live in Bayonne! Of
course, Medicare will only pay what Medicare pays, but if you have most types
of commercial insurance (not to mention, of course, if you are uninsured), it
is another story. To guard against excessively inflated charges, most insurers
have contracts with providers (hospitals, doctors, etc.) that determine how
much they will pay for a procedure or treatment of a disease. This saves the
insurer money. In addition, in order to encourage you to go somewhere that they
have negotiated these lower rates, “in-plan” hospitals, they pay a lower
percent of the cost – and you pay more – if you go “out of plan”.
And it is
precisely this effort to control costs that many for-profit hospitals (like
Bayonne) have turned on its head to generate greater income. They have gone
“out of plan” for all health plans. This means that when you show up in their
ER, or are admitted, you have a higher co-pay, and co-insurance charge, and the
insurer pays them more money. Which is why the insurer doesn’t want you to go
there, and you might (once you knew this) not want to go there either. Except,
of course, you’re sick, and you live in Bayonne, and it is the closest ER. Talk
about gaming the system!
Spending & Coverage (2010)
|
France
|
U.S.
|
Total health spending per capita
|
$3,974
|
$8,233
|
Government health spending per capita
|
$3,061
|
$3,967
|
% uninsured
|
0%
|
15.7%
|
Health
outcomes (2010)
|
||
Life expectancy at birth (2011)
|
81.3 yr.
|
78.7 yr.
|
Infant mortality per 1,000 births
|
3.6
|
6.1
|
Costs
per episode (2012)
|
||
Doctor’s office visit
|
$30
|
$95
|
Hospital day
|
$853
|
$4,287
|
Angioplasty
|
$7,564
|
$28,182
|
Appendectomy
|
$4,463
|
$13,851
|
Childbirth delivery (normal)
|
$3,541
|
$9,775
|
Hip replacement
|
$10,927
|
$40,364
|
Heart bypass
|
$22,844
|
$73,420
|
Tests
(2012)
|
||
Abdominal CT scan
|
$183
|
$630
|
Angiogram
|
$264
|
$914
|
MRI
|
$363
|
$1,121
|
Name-brand
drugs (30-day prescription, 2012)
|
||
Cymbalta
|
$47
|
$176
|
Lipitor
|
$48
|
$124
|
Nexium
|
$30
|
$202
|
Sources:
Organisation for Economic Co-operation and Development and International
Federation
of Health Plans. |
||
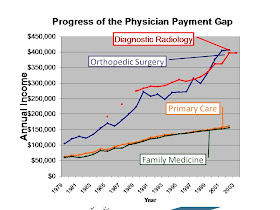
I have implied
that much of the reason for the high cost of health care in the US is the high
cost of procedures. Frankly, that is true. It is why procedural specialists
make so much more than primary care physicians. This is why decreasing the
difference in income potential for proceduralists and primary care doctors
would be good for everyone and save money: there would be more people doing
primary care and less incentive to do unnecessary procedures. Consumers Report, in its July 2013
issue, has an article on the patient-centered medical home (PCMH) movement,
which seeks to achieve the “triple aim” of higher quality, greater patient
satisfaction, and lower cost. The article, “A doctor’s office that’s all about you”, also addresses the high cost of care in
the US, comparing it specifically to France, which spends 11.6% of its GDP on
health care and “…is generally
acknowledged as having one of the world’s best health care systems.” Needless
to say, the comparison is not flattering to the US, which spends 17.6% of GDP
on health care.
Richard Wender, MD, a leader in US family medicine,
commenting on the “Colonoscopies” article, says “Using health care as a driver of corporate economics as opposed to a
public good is the fundamental cause of our medical inflation.” Lee Green,
MD, an American who is now a family medicine leader in Canada, adds “Having practiced most of my career in the
US, and now practicing in Canada, the contrast is quite evident. The US health
care system is not designed to get you the care you need, it is designed to get
you the care that someone can make a profit giving you. If you're poor and
uninsured, that's none - no matter how much you need it. If you're
well-insured, it's a lot - including quite a bit you don't need, and even some
that is harmful.”
This is crazy. We know the problem, and we know the solutions. All we need
is the will to implement them. Maybe this continued exposure will generate it.
We can hope so.