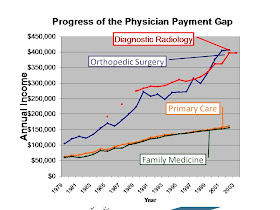
 On February 2, 2011, I posted a piece
titled Outing
the RUC: Medicare reimbursement and Primary Care, describing the activities
of this group, officially the “Specialty Society Relative Value Scale Update
Committee” but known as the RUC, which is convened annually by the American
Medical Association (AMA) to set the relative value of different kinds of work
done by doctors. I included the accompanying graph, from the Robert Graham
Policy Research Center of the American Academy of Family Physicians (AAFP). It
shows the relative income of different specialists over time (FPs are the line
at the bottom) and suggested that this might well impact specialty choice by
students. I noted that the reason for the income disparities was the different
weight given the work done by different specialists, and that the RUC was
dominated by subspecialty societies. I pointed out that the real problem is
that this encourages expensive procedures (by making them expensive) and that
this skews the entire health care system.
On February 2, 2011, I posted a piece
titled Outing
the RUC: Medicare reimbursement and Primary Care, describing the activities
of this group, officially the “Specialty Society Relative Value Scale Update
Committee” but known as the RUC, which is convened annually by the American
Medical Association (AMA) to set the relative value of different kinds of work
done by doctors. I included the accompanying graph, from the Robert Graham
Policy Research Center of the American Academy of Family Physicians (AAFP). It
shows the relative income of different specialists over time (FPs are the line
at the bottom) and suggested that this might well impact specialty choice by
students. I noted that the reason for the income disparities was the different
weight given the work done by different specialists, and that the RUC was
dominated by subspecialty societies. I pointed out that the real problem is
that this encourages expensive procedures (by making them expensive) and that
this skews the entire health care system.
I did not, however, call the RUC “The
shadowy cartel that controls Medicare”. No, that is the title of a lengthy
recent investigative piece in the Washington
Monthly by Haley Sweetland Edwards that documents, in detail, the creation,
formation, function, and results of the RUC’s activities that justifies this
sobriquet. The problems documented are profound. Medicare has to pay for the
work that doctors do, and it is pretty obvious that performing heart surgery
should be paid more than freezing a wart. But how much more? And how does that
relate to your doctor’s office visit or doing and interpreting a CT scan? And
that doctor’s visit; is it for a cold or to manage 5 different chronic
diseases? It’s complicated stuff. So the Center for Medicare and Medicaid
Services (CMS) relies (90% of the time or more) on the recommendations of the
AMA-convened RUC.
Note, above, that in the full name of the RUC the term “specialty
society” is included; the members of the RUC are appointed by medical specialty
societies, but are then told to then be completely objective and not look out
for the interests of those societies, the specialists, or themselves! “Put your
RUC hat on,” Edwards describes the chair of the committee telling its members,
But even if you believe that this is possible, the outcome of RUC decisions
would demonstrate that it is not in fact the case (“…in talking to a half-dozen current and former RUC members, including
both generalists and specialists, the image of the committee that emerges is
less a gathering of angels, cloaked by some Rawlsian Veil of Ignorance, and
more akin to a health care-themed Game of Thrones.”) While the RUC only
makes recommendations for Medicare, because all other payers base their payment
rates upon Medicare, it is essentially controlling the cost of the entire
health care system.
Medicare spending is like a pie, a fixed amount of dollars
divided up based upon RUC recommendations. The original basis for this
division, the Resource Based Relative Value Scale (RBRVS), developed by William
Hsiao, may not have been equitable for primary care, but the modifications
since then have been a disaster. When the first Bush administration gave the
task of making these decisions to the AMA, “…the most powerful interest group in the industry,” Hsaio says “…that was the point where I knew the system
had been co-opted….It had become a political process, not a scientific
process.”

 Edwards
goes on, in great detail, to show the ways that the AMA maintains power – and
makes lots of money – by controlling
the RUC and the charge codes that are associated with it. And also describes,
in detail, how it has a negative impact on primary care (“These manipulated prices are also a major reason why specialists are
in oversupply in many parts of the country, while a worsening shortage of
primary care providers threatens the whole health care delivery system. It’s
precisely because the RUC has overvalued certain procedures and undervalued
others that radiologists now make twice what primary care docs do in a
year—that’s an average of $1.5 million more in a lifetime”) and why (“While the primary care docs make up
roughly 40 percent of physicians nationwide, they have only 14 percent of the
votes on the RUC.”). I would argue with the math, though; over a 30-year
career every $100,000 of additional annual income results in an additional $3
million in lifetime income, and many sub-specialists earn several times
$100,000 more than primary care doctors.
Edwards
goes on, in great detail, to show the ways that the AMA maintains power – and
makes lots of money – by controlling
the RUC and the charge codes that are associated with it. And also describes,
in detail, how it has a negative impact on primary care (“These manipulated prices are also a major reason why specialists are
in oversupply in many parts of the country, while a worsening shortage of
primary care providers threatens the whole health care delivery system. It’s
precisely because the RUC has overvalued certain procedures and undervalued
others that radiologists now make twice what primary care docs do in a
year—that’s an average of $1.5 million more in a lifetime”) and why (“While the primary care docs make up
roughly 40 percent of physicians nationwide, they have only 14 percent of the
votes on the RUC.”). I would argue with the math, though; over a 30-year
career every $100,000 of additional annual income results in an additional $3
million in lifetime income, and many sub-specialists earn several times
$100,000 more than primary care doctors.
The idea of having independent, non-governmental, groups
advise on policy is not necessarily a bad one. An excellent example of this is
the US Preventive Services Task Force (USPSTF), which makes recommendations,
based on the scientific evidence, about which preventive tests are effective
and which are not. In Guidelines,
bias, and your health, June 30, 2013, I cite an article by 2 USPSTF members
who are concerned that by tying payment for services to positive
recommendations by USPSTF, the Affordable Care Act (ACA, “Obamacare”) could
politicize their work. The RUC has no such compunctions. While USPSTF is
intentionally composed mostly of primary care physicians and examines only the
scientific evidence, the RUC is dominated by specialists, who are appointed by
specialty societies, who have a great financial stake in its decisions. And if
the cartoons attached depict the doctors as poker players, the AMA is the “house”, which not
only takes a cut of all decisions, but owns them and sells them back to anyone
who wants to use them.
Edwards’ article is full of quotes from important –
especially those who were formerly important
in public life, both Republican (e.g., Gail Wilensky and Thomas Scully, heads
of CMS during the GHW Bush and GW Bush administrations respectively) and
Democratic (e.g., Bruce Vladeck, who headed CMS under Clinton), who are
extremely critical of the entire process behind the RUC, see it as corrupt, and
see it as a major contributor to a US health system that spends incredible
amounts of money in a wrong-headed, upside-down way to reach mediocre health
outcomes. Unfortunately, none of them changed it when they had government power
(if they even tried to).
I would like to add two notes:
- All specialists are not paid the same. Some (e.g, psychiatrists, some subspecialty pediatricians, some neurologists) are earn much the same as primary care doctors. Some (e.g., radiologists, orthopedic surgeons, neurosurgeons, anesthesiologists) earn several times more. Much of this is built into the RBRVS, which vastly overvalues procedures compared to cognitive care, and exacerbated by the RUC.
- The last time I wrote about the RUC, I received a response from the AMA (AMA response to "Outing the RUC", February 5, 2011). It said "The entire premise of this column is false.” If you wish, you can read my reply in that blog piece. Nice to know they read it.
Yuur summary comments are as clear and concise as I have ever read!
ReplyDeleteThanks!
Cool!
ReplyDelete