The goal for our national policy should be that every person
have the best health status that they can. One component of this, although
certainly not all of it, is access to high-quality appropriate health care
services. This means that people can receive the care that they need, when they
need it, and do not receive unnecessary or harmful care. Access includes both
financial and physical (geographic) access, and also access to high-quality care (see, for example, "Et qui vendit pellucidum", a recent blog post by my friend Dr. Allen Perkins).
One part of having access is that there need to be
sufficient numbers of providers, appropriately trained and distributed to meet
those health needs. It also means that those providers should have no reason or
incentive to preferentially provide certain types of care rather than others,
or care to certain people rather than others. Unfortunately, the profit motive
skews this in the US; we have redundancy of profitable services like “cancer
centers” and “heart centers” in major metropolitan areas, with hospitals
competing for the same pool of patients, while in other areas even primary care
is unavailable. We have excess capacity in some areas (every hospital, for
example, needs an MRI or patients might go somewhere else, even if the number
of MRI scans the population needs doesn’t justify it; providers prefer to take
care of less-complex patients – a single joint replacement in an otherwise-healthy
45 year old with an athletic injury is more profitable than, and thus
preferable to, doing a joint replacement in an 80 year old with multiple
medical problems).
A recent survey of primary care providers in 10 countries by
the by Robin Osborn and colleagues from the Commonwealth Fund, “Primary
Care Physicians In Ten Countries Report Challenges Caring For Patients With
Complex Health Needs”[1],
published in the December 2015 issue of Health
Affairs (only the abstract is available free on line) sought to determine
whether primary care physicians (there are, at least in the US, other providers
like NPs and PAs who are not physicians) feel competent to provide various
types of care. The 10 countries were all wealthy and highly developed (Australia,
Canada, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the
United Kingdom, and the United States). All but the US have some form of
universal health care, although the way that it is organized (e.g., single-payer
government health insurance in Canada, a national health service in the UK,
multiple non-profit insurers in several others) varies from country to country.
In most countries, “primary care” meant family physicians or GPs, but in others
(including the US), it also included general internists and general
pediatricians.
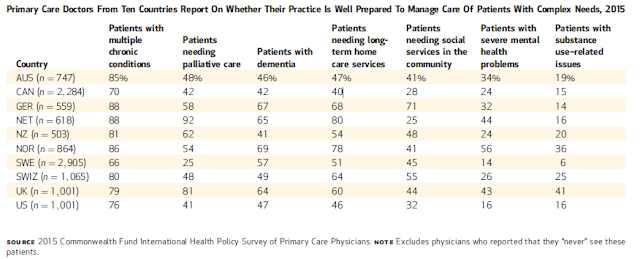
The researchers found both similarities and differences by
country in the percent of primary care practices that had confidence in their
ability to adequately address population health needs, especially those that
are increasing because of the aging of the population. For example, the confidence
of these practices in managing patients with multiple chronic conditions was generally
high (from 70% in Canada to 88% in Germany and the Netherlands; the US was at 76%).
Fewer practices were confident in other areas, and there was greater variance.
For example, 92% of practices in the Netherlands and 81% in the UK had high confidence
in providing palliative care, while Sweden (25%), the US (41%), and Canada
(42%) were much lower. Similar variations existed for other services (see table); for example, confidence in
dealing with patients with substance use related issues were much lower (from 16%
in the US to 41% in the UK).
The authors also surveyed whether practices had a number of
characteristics that many experts think are important for being able to
effectively and efficiently manage complex patients. These included use of
electronic health records (European countries were ahead, but the US and
Canada, late adopters, are catching up), team based care, after hours care not
requiring visiting the ER (the US is very low), access of patients to their
medical records (the US is very high as this is one of the criteria for “meaningful
use” payments from the federal government), communication between different
hospitals, specialists, and ERs with the primary providers (all over the board
including in the US), and many other areas.
Of course, these surveys reflect the experiences of
physicians in different countries, and are thus subjective rather than compared
to some iconic “gold standard”. People do not know what they do not know, or
haven’t experienced, or cannot even imagine; their experiences are
context-dependent, and so cannot be directly compared. For example, the survey
asked whether physicians thought that (their) “system works well; only minor
changes needed”. Only 16% of US doctors
answered positively, with the high being in Norway, 67%. However, in the UK the
number was also very low – 22%. How can we interpret that? In all of these
countries, save the US, including the UK, everyone is covered. 78% of UK
physicians may not believe that their “system works well; only minor changes
needed”, but what would they think if the alternative was a non-system like the
US where there are large numbers of uninsured people? Would they think that a
better system? Probably not, but can’t tell from this data.
Finally, and perhaps most important, the survey does not
look at whether there are a sufficient number and appropriate distribution of
primary care providers to meet a country’s needs even when the practices are
well-organized. It is my impression that the answer to this question is closer
to “enough” in most of these other countries; I am certain it is not in the US.
In our country, the financial rewards for subspecialization and the “lifestyle”
(and sometimes financial) rewards for urban location are major determinants in
our distribution of providers across specialties and geography. There are far
too few primary care providers as a percentage of all physicians, and while family
physicians are far more equitably distributed than other specialists, there are
still big geographic disparities. Among the many “solutions” that have been
suggested, I believe that only one will work: eliminate, or at least
dramatically decrease, the income differential between primary care and
subspecialties. This is not as far-fetched as it seems; as I have discussed
before, high income for some specialists and procedures are not market-drive
but are set by policy; Medicare sets these rates.
As far as geographic disparity is concerned, this is an
issue that most effects primary care and a few other specialties (psychiatry,
general surgery) since most subspecialists practice only in urban areas where
there are sufficient populations to use their services. This also can be
addressed by money: pay providers differentially more for more rural practice.
We also need to provide financial resources to support these practices not only
for income, but for wrap-around care.
A general practitioner from Denmark (not one of the 10
countries surveyed) told me about how his anesthesiologist son-in-law really
liked his work. I chuckled about how much he must make. He told me no, actually
in Denmark GPs make more. This is a good illustration of how our assumptions
are context bound.
It is also the way we need to go in the US.
[1]
Osborn R, Moulds D, Schneider EC, et al., “Primary Care Physicians In Ten
Countries Report Challenges Caring For Patients With Complex Health Needs”, Health Affairs 34, no.12
(2015):2104-2112, doi:
10.1377/hlthaff.2015.1018
1 comment:
Dear Josh,
Greetings from NW England, UK: I've been following your blog for quite a while. Your coverage of medicine and social justice helps demonstrate the scope and utility of Hodges' model a generic conceptual framework I am studying. The plan is to create a new website using a technology enhanced learning approach.
I'll add you to my list on "Welcome to the QUAD"
http://hodges-model.blogspot.co.uk/
There are posts there that illustrate the model's use and how it can support reflection and integration of diverse - complex concepts including policy within a global health context.
Thanks for your time.
Kind regards,
Peter Jones
@h2cm
Post a Comment